Rationale:
Sickle cell disease (SCD) is a genetic hemoglobinopathy characterized by hypercoagulability and accelerated mortality. Venous thromboembolism (VTE) occurs in 11-12% of SCD patients by age of 40 and increases mortality risk two to three-fold. Transthoracic echocardiography (TTE) can identify mortality risk factors in SCD including an elevated tricuspid regurgitant jet velocity (TRV) and diastolic dysfunction. We sought to characterize longitudinal changes in left and right sided cardiac function and to identify the impact of VTE in this process.
Methods:
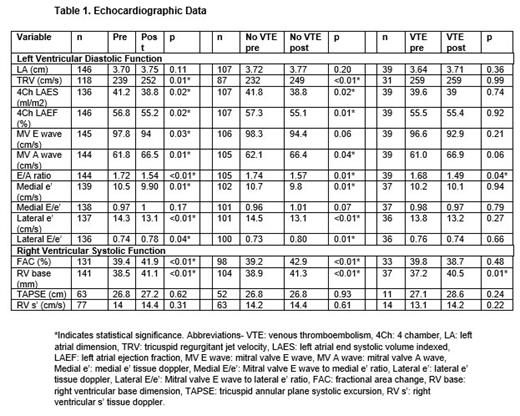
We conducted a retrospective review of 402 consecutive SCD adults, 18 years of age and older, treated at our institution between 2003 and 2021. Deep venous thrombosis and/or pulmonary embolism with confirmatory diagnostic imaging defined VTE. Demographics, clinical history, laboratory data, and diagnostic evaluation were abstracted from the medical record. For echocardiographic data, clinical echocardiograms were individually re-analyzed with extensive coding of left ventricular (LV) and right ventricular (RV) systolic and diastolic function. Data were recorded at time of first contact or prior to VTE if applicable and were repeated at five years post-VTE. In the non-VTE group, baseline and five-year longitudinal data were obtained.
Results:
Within our cohort, 62% were HbSS/HbSβ 0, 56% were female, and 19% had a prior VTE. Prior history of acute chest syndrome, stroke, surgical splenectomy, and avascular necrosis was more common in the VTE group (p<0.01 for each comparison). Mortality was significantly higher in the VTE group compared to the non-VTE group (13% v 6%, p=0.04). In our cohort, 146 patients had initial and 5-year follow-up echocardiography (107/329 of non-VTE group, 39/75 of VTE group). Longitudinally, there were significant declines in both medial e ‘ and lateral e’ velocity and the E/A ratio, reflective of worsening left ventricular diastolic dysfunction. Right-sided cardiac function also worsened with a significantly increased TRV and right ventricular base dimension in follow-up echocardiograms. Of note, the baseline TRV was higher in the VTE group compared to the non-VTE group. In the VTE group, E/A ratio significantly decreased and RV base dimension significantly increased on follow-up study. In the non-VTE group, significant increases in TRV and RV base dimension were observed along decreases in left atrial ejection fraction, medial and lateral e', and E/A ratio on follow-up study (Table 1).
Conclusions:
Patients with SCD and VTE have increased mortality compared to those without VTE. Echocardiography demonstrates longitudinal worsening of left ventricular diastolic and right-sided cardiac function. These changes were more pronounced in the non-VTE group, and the lack of changes in the VTE group may reflect missing data. Our findings need to be confirmed prospectively but suggest the importance of a deeper evaluation of echocardiography to better understand the progression of SCD related cardiac dysfunction and pulmonary hypertension.
Disclosures
Cohen:Forma Therapeutics: Consultancy, Other: member of a one-time advisory board meeting about clinical trial endpoints ; Sanofi: Other: Member of an independent data safety monitoring board. Klings:Novo Nordisk: Consultancy, Other: clinical trial support; Forma: Consultancy, Other: clinical trial support; Novartis: Consultancy, Other: Clinical trial support; United Therapeutics: Consultancy, Other: Clinical trial support; Bayer: Consultancy, Other: clinical trial support; Vertex: Other: Advisory board for gene therapy; CSL Behring: Other: safety review committee for Phase 1 trial.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal